Committee on Practice Bulletins—Gynecology
(Replaces Practice Bulletin Number 108, October 2009)
Make This Small Caps
Make This Small Caps
Polycystic ovary syndrome (PCOS) is a disorder characterized by hyperandrogenism, ovulatory dysfunction, and polycystic ovaries. Its etiology remains unknown, and treatment is largely symptom based and empirical. PCOS has the potential to cause substantial metabolic sequelae, including an increased risk of diabetes and cardiovascular disease, and these factors should be considered when determining long-term treatment. The purpose of this document is to examine the best available evidence for the diagnosis and clinical management of PCOS. Appendix A Table 1
Background
Incidence, Definition, and Diagnostic Criteria
There is no universally accepted definition of PCOS and expert generated diagnostic criteria have proliferated in recent years (see Table 1. The Rotterdam criteria, which supplanted the National Institutes of Health (NIH) diagnostic criteria 1, incorporated the appearance of the ovary based on ultrasound examination into the schema 2. Ultrasound criteria for the diagnosis of polycystic ovaries were decided by expert consensus (see Box 1 3. These criteria have been criticized for including more mild phenotypes, which increases the prevalence of PCOS and may complicate treatment decisions. The Androgen Excess Society (AES) criteria recognize hyperandrogenism as a necessary diagnostic factor, in combination with other symptoms of the syndrome 4. Hyperandrogenism can be established on the basis of clinical findings (eg, hirsutism or acne) or serum hormone measurement. All diagnostic approaches recommend that secondary causes (such as adult-onset congenital adrenal hyperplasia, hyperprolactinemia, and androgen-secreting neoplasms) should first be excluded. All diagnostic schemes also require more than one sign or symptom Table 1, Box 3. Polycystic ovaries alone, for example, are a nonspecific finding and also are frequently noted in women with no endocrine or metabolic abnormalities. Insulin resistance has been noted consistently among many women with PCOS, especially in those with hyperandrogenism, but it is not included in any of the diagnostic criteria 5.
Cannabis sativa (marijuana) is the illicit drug most commonly used during pregnancy. The self-reported prevalence of marijuana use during pregnancy ranges from 2% to 5% in most studies but increases to 15–28% among young, urban, socioeconomically disadvantaged women 0102030405. Higher rates of use are found when querying women at the time of delivery rather than at prenatal visits because some users may not seek prenatal care 5. Notably, 34–60% of marijuana users continue use during pregnancy, with many women believing that it is relatively safe to use during pregnancy and less expensive than tobacco 3, 4, 6,7). A recent study noted that 18.1% of pregnant women reporting marijuana use in the past year met criteria for marijuana abuse, or dependence, or both. 8. A growing number of states are legalizing marijuana for medicinal or recreational purposes, and its use by pregnant women could increase even further as a result.
Make This Small Caps
Make This Small Caps
Table 1.
Recommended Diagnostic Schemes for Polycystic Ovary Syndrome by Varying Expert Groups
Box 1.
Suggested Evaluation for Patients With Polycystic Ovary Syndrome
Physical
-
Blood pressure
-
BMI (weight in kilograms divided by height in meters squared)
-
○ 25–30 = overweight, greater than 30 = obese
-
-
Waist circumference to determine body fat distribution
-
○ Value greater than 35 inches = abnormal
-
-
Presence of stigmata of hyperandrogenism and insulin resistance
-
○ Acne, hirsutism, androgenic alopecia, acanthosis nigricans
-
Laboratory
-
Documentation of biochemical hyperandrogenemia
-
○ Total testosterone and sex hormone-binding globulin or bioavailable and free testosterone
-
-
Exclusion of other causes of hyperandrogenism
-
○ Thyroid-stimulating hormone levels (thyroid dysfunction)
-
○ Prolactin (hyperprolactinemia)
-
○ 17-hydroxyprogesterone (nonclassical congenital adrenal hyperplasia due to 21 hydroxylase deficiency)
-
— Random normal level less than 4 ng/mL or morning fasting level less than 2 ng/mL
-
-
○ Consider screening for Cushing syndrome and other rare disorders such as acromegaly
-
-
Evaluation for metabolic abnormalities
-
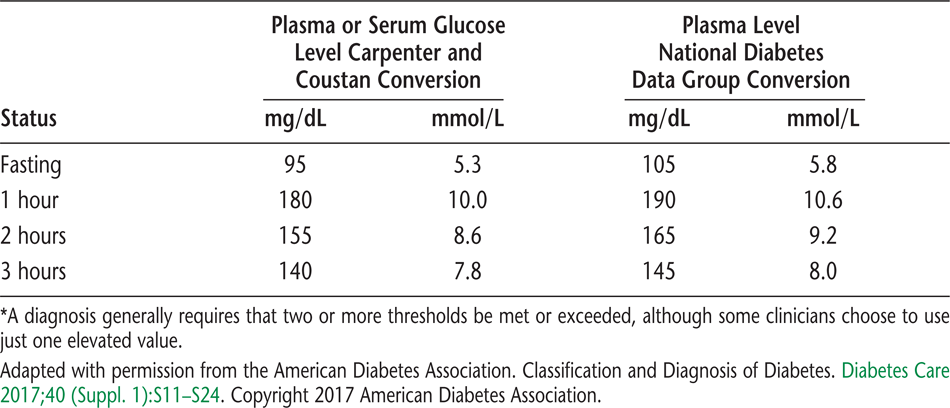
○ Two-hour oral glucose tolerance test (fasting glucose less than 110 mg/dL = normal, 110–125 mg/dL = impaired, greater than 126 mg/dL = type 2 diabetes) followed by 75 g oral glucose ingestion and then 2-hour glucose level (less than 140 mg/dL = normal glucose tolerance, 140–199 mg/dL = impaired glucose tolerance, greater than 200 mg/dL = type 2 diabetes)
-
-
Fasting lipid and lipoprotein level (total cholesterol, high-density lipoproteins less than 50 mg/dL abnormal, triglycerides greater than 150 mg/dL abnormal [low-density lipoproteins usually calculated by Friedewald equation])
Ultrasound Examination
-
Determination of polycystic ovaries: in one or both ovaries, either 12 or more follicles measuring 2–9 mm in diameter, or increased ovarian volume (greater than 10 cm3). If there is a follicle greater than 10 mm in diameter, the scan should be repeated at a time of ovarian quiescence in order to calculate volume and area. The presence of one polycystic ovary is sufficient to provide the diagnosis.
-
Identification of endometrial abnormalities
Optional Tests to Consider
-
Gonadotropin determinations to determine cause of amenorrhea
-
Fasting insulin levels in younger women, those with severe stigmata of insulin resistance and hyperandrogenism, or those undergoing ovulation induction
-
Twenty-four hour urinary free-cortisol excretion test or a low–dose dexamethasone suppression test in women with late onset of polycystic ovary syndrome symptoms or stigmata of Cushing syndrome
Box 2.
Metabolic Syndrome
The metabolic syndrome in women most commonly is diagnosed by the updated Adult Treatment Panel III criteria of an elevated blood pressure level (greater than or equal to 130/85), increased waist circumference (greater than or equal to 35 inches), elevated fasting glucose levels (greater than or equal to 100 mg/dL), reduced high-density lipoprotein cholesterol level (less than or equal to 50 mg/dL), and elevated triglyceride levels (greater than or equal to 150 mg/dL).
Data from Grundy SM, Cleeman JI, Dariels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute scientific statement: executive summary. Circulation 2005;112:e285–e290.
The incidence of PCOS varies according to the diagnostic criteria. Women with hyperandrogenic chronic anovulation (ie, NIH criteria) make up approximately 7% of reproductive-aged women. There are no significant differences in the prevalence of hirsutism or elevated circulating androgen levels between white and black women 6. The broader Rotterdam criteria increase the prevalence of PCOS in women with normogonadotropic anovulation to 91% from 55% using the NIH criteria 7. The prevalence according to the AES criteria will fall between these values 4.
Etiology
The genetic contribution to PCOS remains uncertain, and there is currently no recommended genetic screening test. No specific environmental substance has been identified as causing PCOS. Insulin resistance may be central to the etiology of the syndrome 5. Obesity is a comorbidity that may amplify the effects of PCOS. However, obesity is not a diagnostic criterion for PCOS, and approximately 20% of women with PCOS are not obese. Obesity is more prevalent in the United States than in other countries and, therefore, the PCOS phenotype may be different. Compensatory hyperinsulinemia may result in decreased levels of sex hormone–binding globulin (SHBG) and, thus, more bioavailable circulating androgen and serve as a trophic stimulus to androgen production in the adrenal gland and ovary. Insulin also may have direct hypothalamic effects, such as abnormal appetite stimulation and gonadotropin secretion. Hyperandrogenism, although central to the syndrome, may have multiple etiologies, some not related to insulin resistance.
Clinical Manifestations
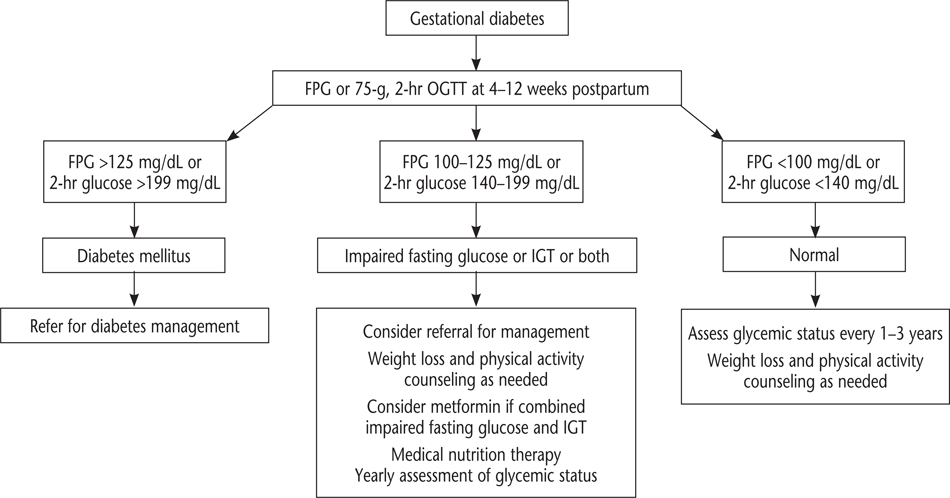
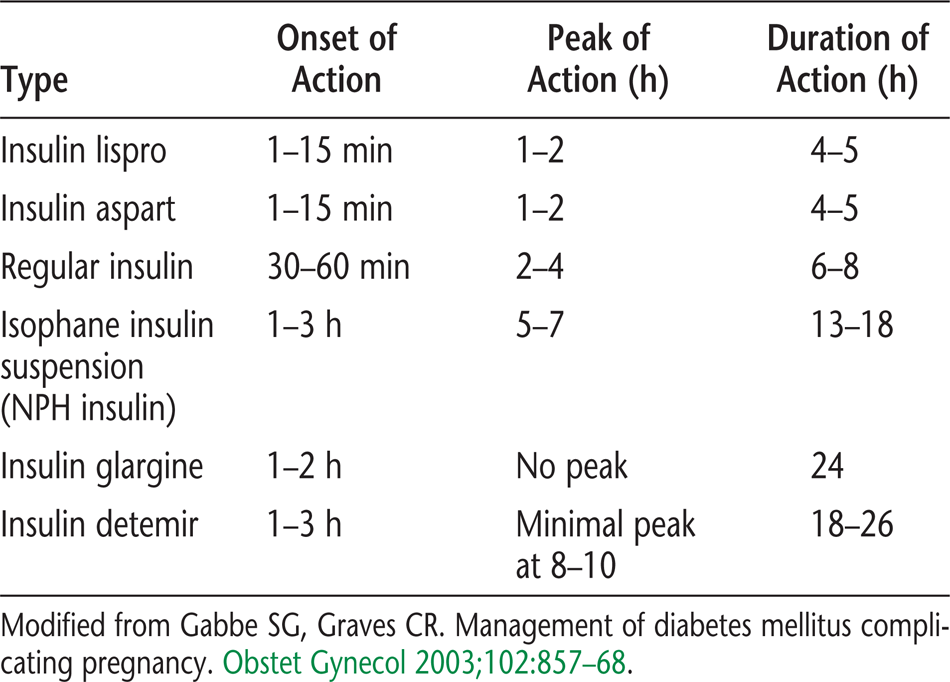
Women with PCOS commonly present with menstrual disorders (from amenorrhea to menorrhagia) and infertility. For this reason, much attention has been focused on the risks of ovulation induction among women with PCOS because they are at increased risk of ovarian hyperstimulation syndrome and multifetal pregnancy. In addition, women with PCOS appear to be at increased risk of complications of pregnancy, including gestational diabetes and hypertensive disorders 8. The risk of complications is further exacerbated by iatrogenic multiple pregnancy from infertility treatment.
Skin disorders, especially those due to peripheral androgen excess such as hirsutism and acne, and to a lesser degree androgenic alopecia, are common in women with PCOS 9. Women with PCOS are at increased risk of insulin resistance and its associated conditions, such as the metabolic syndrome (see Box 2 10, nonalcoholic fatty liver disease 11, and obesity-related disorders such as sleep apnea 12. In turn, all of these conditions are risk factors for long-term metabolic sequelae, such as type 2 diabetes and cardiovascular disease. Women with PCOS also have multiple risk factors for endometrial cancer, including chronic anovulation, centripetal obesity, and diabetes, although the strength of the association with PCOS per se is debated 13. In recent years, there has been increased recognition of mood disturbances and depression among women with PCOS 14.
Box 3.
Factors to Consider in the Differential Diagnosis of Polycystic Ovary Syndrome
-
Androgen secreting tumor
-
Exogenous androgens
-
Cushing syndrome
-
Nonclassical congenital adrenal hyperplasia
-
Acromegaly
-
Genetic defects in insulin action
-
Primary hypothalamic amenorrhea
-
Primary ovarian failure
-
Thyroid disease
-
Prolactin disorders
Liver Injury
Most patients with drug-induced liver injury who survive the initial injury recover completely 36. After drug discontinuation, liver injury may occasionally worsen before improvement is noticed 13.
Most patients who develop subclinical ALT elevations recover without sequelae 14. The course of resolution can be variable but generally occurs over weeks to months. Cholestatic injury will improve over several months with discontinuation of the medication. Occasionally, complete resolution of cholestatic injury may take up to 1 year after drug removal 13. Hepatic tumors associated with drug therapy typically are benign and also resolve when the medication is discontinued 37. After drug withdrawal, patients should be monitored with repeated biochemical measurements.
Consultation with a specialist should be considered in patients with bilirubin levels greater than twice the upper limit of normal and an ALT level greater than three times the upper limit of normal because these levels may indicate a poor prognosis 13, 14. Additionally, when the diagnosis is in question or the presentation is severe, referral to a specialist or admission to a hospital may be warranted.
Drug-induced liver injury typically is not treated with additional medications. However, a few exceptions exist. N-acetylcysteine is used for acetaminophen toxicity 13 and has been studied in nonacetaminophen causes of drug-induced liver injury 36. Intravenous (IV) carnitine is administered in cases of valproate overdose 13. Corticosteroids are used for immune-mediated reactions and ursodeoxycholic acid for cholestatic drug-induced liver injury, although this remains controversial 11, 13.
This patient is having vague symptoms that may suggest liver disease. Her initial workup should include obtaining a full medication history, including OTC medications, herbal products, and recently discontinued medications. A complete medical history and laboratory test results were obtained. The results are as follows: ALT level, 500 units per liter; aspartate transaminase level, 100 units per liter; alkaline phosphatase level, 180 units per liter; and total bilirubin level, 1.5 mg/dL. The calculated R value is 6. Imaging studies, usually ultrasonography and computed tomography, also are performed. Acute hepatocellular injury is diagnosed based on the medications and the timing of starting the medications. Because lisinopril and simvastatin were started simultaneously and both are known to cause this type of liver injury, both medications are stopped and referral to a specialist should be considered because of the high ALT and alkaline phosphatase levels.
Differential Diagnosis of PCOS
The differential diagnosis of PCOS includes other causes of androgen excess (see Box 3. The essential components of the history and physical examination necessary to diagnose the underlying cause of the disorder are described in Box 1. The history should focus on the onset and duration of the various signs of androgen excess, the menstrual history, and concomitant medications, including the use of exogenous androgens. A family history of diabetes and cardiovascular disease (especially first-degree relatives with premature onset of cardiovascular disease [male younger than 55 years and female younger than 65 years]) is important.
The physical examination should include evaluation of balding, acne, clitoromegaly, and body hair distribution, as well as pelvic examination to look for ovarian enlargement. The presence and severity of acne should be noted. Signs of insulin resistance such as hypertension, obesity, centripetal fat distribution, and the presence of acanthosis nigricans should be recorded. Acanthosis nigricans is a dermatologic condition marked by velvety, mossy, verrucous, hyperpigmented skin. It has been noted on the back of the neck, in the axillae, underneath the breasts, and even on the vulva. The presence of acanthosis nigricans appears to be more a sign of insulin resistance or medication reaction than a distinct disease unto itself. Other pathologic conditions rarely associated with acanthosis nigricans should be considered, such as insulinoma and malignant disease, especially adenocarcinoma of the stomach. Clitoromegaly is rarely associated with PCOS, and its presence should elicit a search for other causes.
Because Cushing syndrome is extremely rare (1 in 1,000,000 individuals) and screening tests are not 100% sensitive or specific 15, routine screening for Cushing syndrome in all women with hyperandrogenic chronic anovulation is not indicated. Those who have coexisting signs of Cushing syndrome, including a moon facies, buffalo hump, abdominal striae, centripetal fat distribution, or hypertension, should be screened (see Box 1. Proximal myopathies and easy bruising, not typically present in women with PCOS, also may help identify patients with Cushing syndrome.
Androgen-secreting tumors of the ovary or adrenal gland are invariably accompanied by elevated circulating androgen levels. However, there is no absolute level that is pathognomonic for a tumor, just as there is no minimum androgen level that excludes a tumor. In the past, testosterone levels above 2 ng/mL and dehydroepiandrosterone sulfate (DHEAS) levels greater than 700 micrograms/dL were regarded as suspicious for a tumor of ovarian and adrenal etiology, respectively, but these cutoff levels have poor sensitivity and specificity 16.
The best measurement of circulating androgens to document unexplained androgen excess is uncertain. The present recommendation by the AES is to measure free testosterone concentration either directly by equilibrium dialysis, or to calculate the free testosterone based on the total testosterone measured accurately (eg, by radioimmunoassay using column chromatography, or by mass spectrometry) and SHBG (eg, measured using competitive binding or a high quality immune-based assay). Each clinician should be familiar with the analytical performance and the normal ranges of local laboratories because there is no standardized testosterone assay in the United States and the sensitivity and reliability in the female ranges are often poor 17. Evaluation of DHEAS levels may be useful in cases of rapid virilization (as a marker of adrenal origin), but its utility in assessing common hirsutism is questionable.
Both the adrenal glands and ovaries contribute to the circulating androgen pool in women. The adrenal gland preferentially secretes weak androgens such as dehydroepiandrosterone (DHEA) or DHEAS (up to 90% of adrenal origin). These hormones, in addition to androstenedione, may serve as prohormones for more potent androgens such as testosterone or dihydrotestosterone. The ovary is the primary source of testosterone, and it is estimated that 75% of circulating testosterone originates from the ovary (mainly through peripheral conversion of prohormones by liver, fat, and skin, but also through direct secretion). Androstenedione, largely of ovarian origin, is the only circulating androgen that is higher in premenopausal women than men, yet its androgenic potency is only 10% of testosterone. Dihydrotestosterone is the most potent androgen, although it circulates in negligible quantities and results primarily from the intracellular 5-α-reduction of testosterone.
Mild elevations in prolactin are common in women with PCOS 18. A prolactin level can identify prolactinomas that secrete large amounts of prolactin and that may stimulate ovarian androgen production, but this is an extremely rare cause of hyperandrogenic chronic anovulation. Evaluating serum levels of thyroid-stimulating hormone also is useful given the protean manifestations and frequency of thyroid disease in women with menstrual disorders.
Clinical Considerations and Recommendations
▸
Nonclassical congenital adrenal hyperplasia, often referred to as late-onset congenital adrenal hyperplasia, can present in adult women with anovulation and hirsutism and is almost exclusively due to genetic defects in the steroidogenic enzyme, 21 hydroxylase (CYP21). In Europe and the United States, congenital adrenal hyperplasia occurs with the highest prevalence among Ashkenazi Jews, followed by Hispanics, Yugoslavs, Native American Inuits in Alaska, and Italians 19. Women in groups at higher risk of nonclassical congenital adrenal hyperplasia and a suspected diagnosis of PCOS should be screened with a 17-hydroxyprogesterone value.
To screen for nonclassical congenital adrenal hyperplasia due to CYP21 mutations, a fasting level of 17-hydroxyprogesterone should be obtained in the morning. A value less than 2 ng/mL is considered normal. If the sample is obtained in the morning and during the follicular phase, some investigators have proposed cutoffs as high as 4 ng/mL 20. Specificity decreases if the sample is obtained in the luteal phase. High levels of 17-hydroxyprogesterone should prompt an adrenocorticotropic hormone (ACTH) stimulation test.
▸
Obesity contributes substantially to reproductive and metabolic abnormalities in women with PCOS. Multiple studies have shown that weight loss can improve the fundamental aspects of the endocrine syndrome of PCOS by lowering circulating androgen levels and causing spontaneous resumption of menses. Reduction in body weight has been associated with improved pregnancy rates and decreased hirsutism, as well as improvements in glucose and lipid levels 21222324. Studies using pharmacologic weight loss agents, such as orlistat, an intestinal inhibitor of lipid absorption, and sibutramine, an anorexic agent, in women with PCOS have shown similar improvement in ovarian function 2526. Morbidly obese women with PCOS who undergo gastric bypass surgery experience near normalization of their reproductive and metabolic abnormalities 27. These changes have been reported with weight loss as little as 5% of the initial weight 28. The decrease in unbound testosterone levels after weight loss may be largely mediated through increases in SHBG 28. The effects of weight loss in normal weight women with PCOS are unknown.
▸
Women with a diagnosis of PCOS should be screened for type 2 diabetes and impaired glucose tolerance with a fasting glucose level followed by a 2-hour glucose level after a 75-g glucose load 29 (see Box 1. Retrospective studies of women with PCOS have noted a twofold to fivefold increased risk of diabetes in women with PCOS when compared with a control population 3031. In a prospective, cohort study, 11.9% of women older than 30 years with PCOS had a physician's diagnosis of type 2 diabetes, compared with only 1.4% of controls 32. Other cohort studies have suggested as many as 40% of U.S. women with PCOS demonstrate glucose intolerance when the less stringent World Health Organization criteria are applied (2-hour glucose levels greater than or equal to 140 mg/dL) 3334, although the prevalence is lower in a thinner European population 35. Undiagnosed diabetes ranges from 3–10% in these PCOS cohorts. The risk factors associated with glucose intolerance in women with PCOS—age, high body mass index (BMI) high waist–hip ratios, and family history of diabetes—are identical to those in other populations.
There is no recommended screening test for insulin resistance. Instead, there has been increasing recognition of the metabolic syndrome, a clinical phenotype of insulin resistance with increased diabetes and cardiovascular disease risk (see Box 2. The metabolic syndrome is common among women with PCOS, affecting 33% of women participating in a large multicenter trial 10.
Fasting glucose levels are poor predictors of glucose intolerance risk in women with PCOS and, thus, some groups recommend adding an oral glucose tolerance test to screening for the metabolic syndrome. This finding has taken on new significance with the findings of the Diabetes Prevention Program and other diabetes prevention trials that both lifestyle interventions and the use of antidiabetic drugs such as metformin significantly reduce the risk of developing diabetes in women with impaired glucose tolerance 36.
There is little utility to routine testing of insulin levels in women with PCOS. Insulin level assessment has not been shown to identify women who will respond to therapy.
▸
Women with PCOS should be screened for cardiovascular risk by determination of BMI, fasting lipid and lipoprotein levels, and metabolic syndrome risk factors (see Box 2 and Box 3). Women with PCOS should be rescreened periodically for cardiovascular disease risk factors because conversion to impaired glucose tolerance approaches 20% per year 37, although low-density lipoprotein (LDL) levels have tended to persist and plateau over time 38. Regular exercise and weight control are proven methods to reduce cardiovascular morbidity and mortality. These modalities should be considered before prescription drugs are used.
Dyslipidemia is a common metabolic abnormality among women with PCOS. The prevalence of borderline or high lipid levels according to National Cholesterol Education Program guidelines approaches 70% in women with PCOS 39. Low-density lipoprotein levels are disproportionately elevated in women with PCOS 3839.
An increased risk and early onset of cardiovascular disease in women with PCOS is strongly suspected but less well documented. No prospective studies have documented an increased risk of cardiovascular events in women with PCOS. However, a number of cohort studies, including the Nurse's Health Study, have suggested an increased dose–response risk of cardiovascular disease or events in the presence of increasing oligomenorrhea 40 or with more symptoms of PCOS in a menopausal population 4142. Studies in premenopausal women with PCOS have detected an increased prevalence of subclinical atherosclerosis compared with controls (ranging from less than 10% in women with PCOS and increased carotid intimal medial thickness to 40% in those with PCOS and coronary artery calcification) 434445.
▸
Combination Hormonal Contraception
There are several options to treat menstrual disorders associated with PCOS. Combination low-dose hormonal contraceptives are most frequently used for long-term management and are recommended as the primary treatment of menstrual disorders. Although there are few well designed trials in women with PCOS, in general, combined hormonal contraceptives offer benefits through a variety of mechanisms, including suppression of pituitary luteinizing hormone secretion, suppression of ovarian androgen secretion, and increased circulating SHBG. Individual preparations may have different doses and drug combinations and thus have varying risk–benefit ratios. For instance, various progestins have been shown to have different effects on circulating SHBG levels 46, but whether that results in a clinical benefit is uncertain. There is insufficient evidence to determine the most effective combination hormonal contraceptive for women with PCOS to treat menstrual disorders.
Progestin
No studies have addressed the long-term use of depot medroxyprogesterone acetate and intermittent oral medroxyprogesterone acetate to treat hirsutism. The regimen of cyclic oral progestin therapy or progestin-containing intrauterine devices that most effectively prevent endometrial cancer in women with PCOS is unknown. Progestin-only contraceptives or progestin-containing intrauterine devices are an alternative for endometrial protection, but they are associated with abnormal bleeding patterns in 50–89% of users 47.
Insulin-Sensitizing Agents
Drugs initially developed to treat type 2 diabetes also have been used to treat PCOS. Most studies initially focused on agents that improve peripheral insulin sensitivity by lowering circulating insulin levels. These agents include biguanides (ie, metformin) and thiazolidinediones (ie, pioglitazone and rosiglitazone) 4849. They are rarely associated with hypoglycemia. These drugs are often referred to as insulin-sensitizing agents, but their individual effects and risk–benefit ratios vary. There are class differences, for example, biguanides tend to decrease weight and thiazolidinediones tend to increase weight. Within a class there also can be significant differences in the risk–benefit ratio 50. These effects have diminished interest in the use of thiazolidinediones to treat PCOS. Nonetheless, improving insulin sensitivity with these agents is associated with a decrease in circulating androgen levels, improved ovulation rate, and improved glucose tolerance 5152.
Because ovulation rates will likely improve with treatment, it is important to discuss contraceptive options. It is difficult to separate the effects of improving insulin sensitivity from those of lowering serum androgens because any improvement in insulin sensitivity can raise SHBG and, thus, lower bioavailable androgen.
None of the antidiabetic agents noted are currently approved by the U.S. Food and Drug Administration (FDA) for treatment of PCOS-related menstrual dysfunction, although metformin appears to have the safest risk–benefit ratio. There are no randomized controlled studies of treatment for 1 year or more with these agents in women, children, or adolescents with PCOS. The effects of these drugs on preventing endometrial hyperplasia or endometrial neoplasia in women with PCOS are largely unknown.
▸
Lifestyle modifications are the best approach to modifying risks for cardiovascular disease and diabetes. Insulin-sensitizing drugs and statins also can be considered.
Lifestyle Modification
An increase in exercise combined with dietary change has consistently been shown to reduce diabetes risk comparable to or better than medication 36. Weight loss may improve metabolic abnormalities associated with PCOS. In terms of weight loss, caloric restriction rather than the composition of the diet is the key factor 53, and smaller trials in women with PCOS have shown no other advantage to a particular hypocaloric diet 54. Thus, there is no ideal dietary modification for women with PCOS beyond caloric restriction.
Insulin-Sensitizing Agents
The Diabetes Prevention Program demonstrated that metformin can delay the development of diabetes in high-risk populations (eg, those with impaired glucose tolerance) 36, and this result has been replicated for a number of antidiabetic drugs in individuals at high risk. Among women with PCOS who use metformin, glucose tolerance improves or stays steady over time 55. Metformin also may be associated with weight loss, but results are inconsistent 52. Metformin is often used in conjunction with lifestyle therapy to treat PCOS. Recent studies suggest that there is little benefit to the addition of metformin above lifestyle therapy alone 5657.
Metformin carries a small risk of lactic acidosis, most commonly among women with poorly controlled diabetes and impaired renal function. Gastrointestinal symptoms (diarrhea, nausea, vomiting, abdominal bloating, flatulence, and anorexia) are the most common adverse reactions and may be ameliorated by starting at a small dose and gradually increasing the dose or by using the sustained-release version now available in the United States. The dose most commonly used to treat women with PCOS is 1,500–2,000 mg per day given in divided doses.
Currently, data are insufficient to recommend insulin-sensitizing agents prophylactically to prevent diabetes in women with PCOS. However, results of diabetes prevention trials may favor more aggressive management when impaired glucose tolerance or metabolic syndrome is present to prevent diabetes.
Statins
Another area where there is emerging support in the literature for a cardiovascular and endocrine benefit in women with PCOS is the use of statins 58. However, their long-term effects in preventing cardiovascular disease in young women, especially adolescent girls, with PCOS is unknown.
Combined Hormonal Contraceptives and Progestins
There is no convincing evidence to demonstrate an increased risk of adverse effects of combined hormonal contraceptives and progestins on diabetes and cardiovascular risk in women with PCOS and, therefore, these agents may be considered. In the general population, hormonal contraceptive use has not been associated with an increased risk of developing type 2 diabetes 59. The use of hormonal contraceptives does not appear to contribute to the risk of diabetes in women with PCOS, although there are often adverse effects on insulin sensitivity that may be dose dependent 6061. Therefore, a low-dose hormonal contraceptive pill is recommended. Oral contraceptives also may be associated with a significant elevation in circulating triglycerides as well as in high-density lipoprotein (HDL) levels, although these do not appear to progress over time 62. There is no evidence to suggest that women with PCOS experience more cardiovascular events than the general population when they use oral contraceptives, although risk factors for adverse events such as hypertension, obesity, clotting history, and smoking must be considered. The effect of progestins alone on metabolic risk factors varies and is not well understood.
▸
There is no evidence-based schema to guide the initial and subsequent choices of ovulation induction methods in women with PCOS. The American Society for Reproductive Medicine and the European Society of Human Reproduction and Embryology (ASRM/ESHRE) recommend that before any intervention is initiated, preconception counseling should emphasize the importance of lifestyle modification (especially weight reduction and exercise in women who are overweight), smoking cessation, and reduction of alcohol consumption 63.
For some time, the recommended first-line treatment for ovulation induction was the antiestrogen clomiphene citrate. However, recent randomized controlled trial data and Cochrane systematic review findings show that the aromatase inhibitor letrozole is associated with increased ovulation rates, clinical pregnancy rates, and live-birth rates compared with clomiphene citrate 6465. If clomiphene citrate or letrozole use fails to result in pregnancy, the recommended second-line intervention is either exogenous gonadotropins or laparoscopic ovarian surgery 63.
All ovulation induction drugs are associated with an increase in multiple births and related obstetric and neonatal risks such as preterm birth and hypertensive disorders. Clomiphene citrate and letrozole are associated with a comparable risk of twin gestation 64. These rates may be even higher in women with PCOS undergoing ovulation induction 63.
Aromatase Inhibitors
Aromatase inhibitors, such as letrozole, have been used off-label and proposed as primary and secondary treatment for ovulation induction. In an early meta-analysis of four published trials that included 662 women with PCOS, pregnancy rates were similar between women treated with clomiphene citrate and women treated with letrozole (relative risk, 1.02; 95% CI, 0.83–1.26) 66. However, in a more recent randomized controlled trial, letrozole was more effective than clomiphene citrate, with a higher live birth rate (27.5% versus 10.1%,
When prescribing letrozole for ovulation induction, patients should be counseled that unlike clomiphene citrate, letrozole is not approved by the FDA for ovulation induction. Letrozole, like clomiphene citrate, is contraindicated for use during pregnancy. If prescribing letrozole, the starting dosage is 2.5 mg/day for 5 days typically starting on day 3, 4, or 5 after a spontaneous menses or progestin-induced bleed. If ovulation does not occur, the dosage can be increased to 5 mg/day for 5 days with a maximum dosage of 7.5 mg/day. Dosages higher than 7.5 mg/day have been associated with thinning of the endometrium as seen with clomiphene citrate 67.
Clomiphene Citrate
Clomiphene citrate has traditionally been the first-line treatment agent for anovulatory women, including those with PCOS, and several multicenter randomized controlled trials have upheld the use of clomiphene citrate as first-line treatment compared with metformin alone or placebo. Six-month live birth rates range from 20% to 40% depending on the population 686970. One half of all women who are going to conceive using clomiphene citrate will do so at the 50-mg starting dose, and another 20% will do so at the 100-mg per day dosage 71. Most pregnancies will occur within the first six ovulatory cycles, although a constant monthly pregnancy rate was noted suggesting there may be continued benefit to longer use 69. Clomiphene citrate is contraindicated for use during pregnancy.
Alternative clomiphene citrate regimens have been developed, including prolonging the period of administration 72, pretreating with oral contraceptives 73, and adding dexamethasone. Dexamethasone as adjunctive therapy with clomiphene citrate has been shown to increase ovulation and pregnancy rates in clomiphene citrate-resistant women with PCOS 74.
Gonadotropins
Gonadotropins are frequently used to induce ovulation in women with PCOS for whom clomiphene citrate treatment has failed. Low-dose therapy with gonadotropins offers a higher rate of ovulation and monofollicular development, with a significantly lower risk of ovarian hyperstimulation syndrome 75. This low-dose regimen is recommended when using gonadotropins in women with PCOS 63.
Ovarian Drilling
The value of laparoscopic ovarian drilling with laser or diathermy as a primary treatment for subfertile women with anovulation and PCOS is undetermined 76, and it is primarily recommended as second-line therapy. Neither drilling by laser nor diathermy has any obvious advantage, and there is insufficient evidence to suggest a difference in ovulation or pregnancy rates when drilling is compared with gonadotropin therapy as a secondary treatment 76. Multiple pregnancy rates are reduced in those women who conceive following laparoscopic drilling. In some cases, the fertility benefits of ovarian drilling may be temporary, and adjuvant therapy after drilling with clomiphene citrate or gonadotropins may be necessary 77. The long-term effects of laparoscopic ovarian drilling on ovarian function are unclear. Ovarian drilling does not appear to improve metabolic abnormalities in women with PCOS 78.
Insulin-Sensitizing Agents
Metformin
The use of metformin alone as first-line infertility therapy has not been supported by randomized trials. Clomiphene citrate is approximately three times more effective at achieving live birth compared with metformin. Meta-analysis has suggested there may be an increase in pregnancy rates by adding clomiphene citrate to metformin, particularly in obese women with PCOS compared with use of clomiphene citrate alone (OR, 2.67; 95% CI, 1.45–4.94; number needed to treat, 4.6) 79. Metformin has no known human teratogenic risk or embryonic lethality in humans and appears safe in pregnancy (it is also classified as Pregnancy Category B). There is no solid evidence that metformin use early in pregnancy prevents pregnancy loss, and the randomized trials that stopped drug use after a positive pregnancy test result have shown similar miscarriage rates with metformin as with clomiphene citrate.
▸
Although medical methods improve hirsutism, they do not produce the dramatic results women desire, and treatment is often palliative rather than curative. Laser therapy is increasingly used. In general, combination therapies appear to produce better results than single-agent approaches. Clinical trials of hirsutism, with the exception of eflornithine HCl facial cream, tend to be small, single center, with incomplete assessment of clinical and patient response to treatment. Therefore, there is no clear primary treatment for hirsutism in PCOS.
Combined Hormonal Contraceptives
No combined hormonal contraceptive has been approved by the FDA for the treatment of hirsutism. A number of observational or nonrandomized studies have noted improvement in hirsutism in women with PCOS who use oral contraceptives, but no studies of adequate power confirm their benefit in improving hirsutism in PCOS 80. Few studies have compared outcomes of different types of combined hormonal contraceptives, and no one type of pill has been shown to be superior in treating hirsutism in women with PCOS. A number of studies have found additive benefit when oral contraceptives are combined with other treatment modalities, most commonly spironolactone. If a combination hormonal contraceptive is used that contains drospirenone, a progestin with antimineralocorticoid properties, it may be necessary to reduce the dose of spironolactone if used as additional therapy and evaluate the woman's potassium levels.
Antiandrogens
None of the antiandrogen agents were developed to treat hyperandrogenism in women or are approved by the FDA for that indication. They have been used empirically in women with PCOS. The quality of trials examining hirsutism has been poor. A recent meta-analysis could only include 12 out of 348 eligible trials 81, and found these agents are mildly effective. These compounds primarily antagonize the binding of testosterone and other androgens to the androgen receptor. Androgen antagonism may result in improvements in other metabolic variables such as improvements in body composition and circulating lipid levels 82. All appear to offer some benefit, although the best choice for hirsutism in PCOS is unknown. As a class, antiandrogens are teratogenic and pose a risk of feminization of the external genitalia in a male fetus (ambiguous genitalia) should the patient conceive. Therefore, they are frequently used in combination with oral contraceptives.
Spironolactone
Spironolactone, a diuretic and aldosterone antagonist, also binds to the androgen receptor as an antagonist. It has other mechanisms of action, including inhibition of ovarian and adrenal steroidogenesis, competition for androgen receptors in hair follicles, and direct inhibition of 5-α-reductase activity. The usual dosage is 25–100 mg, twice a day, and the dose is titrated to balance efficacy while avoiding side effects such as orthostatic hypotension. A full clinical effect may take 6 months or more. Approximately 20% of women using spironolactone will experience increased menstrual frequency 83. Because it can cause and exacerbate hyperkalemia, spironolactone should be used cautiously in women with renal impairment. Rarely, exposure has resulted in ambiguous genitalia in male infants.
Flutamide
Flutamide, an androgen-receptor agonist, is another nonsteroidal antiandrogen that has been shown to be effective against hirsutism in smaller trials. The most common side effect is dry skin, but its use has been associated with hepatitis in rare cases. The common dosage is 125–250 mg/d. The risk of teratogenicity with this compound is significant, and contraception should be used. Flutamide also has been combined with lifestyle and metformin therapy for treatment of PCOS and may have additive effects 82.
Finasteride
Finasteride inhibits both forms of the enzyme 5-α-reductase (type 1, predominantly found in the skin, and type 2, predominantly found in the prostate and reproductive tissues). It is available as a 5-mg tablet for the treatment of prostate cancer and a 1-mg tablet for the treatment of male alopecia. Finasteride is better tolerated than other antiandrogens, with minimal hepatic and renal toxicity; however, it has a well-documented risk of teratogenicity in male fetuses, and adequate contraception should be used.
Insulin-Sensitizing Agents
There are few data to support the efficacy of metformin in the treatment of hirsutism 80. In a proof of concept 44-week study of an insulin sensitizer, only the highest dose of troglitazone (a thiazolidinedione now removed from the market) was found to significantly—although only modestly—improve hirsutism in women with PCOS 51. Studies with better precision and longer duration are needed to detect differences between classes of insulin-sensitizing agents and their long-term benefits. Currently, there is little or no clear benefit to the use of insulin-sensitizing agents 84.
Eflornithine
An inhibitor of the enzyme ornithine decarboxylase, topical eflornithine has been approved by the FDA for treating female facial hirsutism. After 6 months of treatment, approximately 60% of women improved and one third were considered a clinical success. Success rates did not appear to have been affected by age and prior hair removal techniques, although a higher success rate was observed in white people than other populations (37% versus 22%), although black people did benefit from treatment. The cream is applied twice a day to affected facial areas. Side effects were primarily local with stinging, burning, erythema, and rarely a rash 85.
▸
Mechanical hair removal (shaving, plucking, waxing, depilatory creams, electrolysis, and laser vaporization) is often the front line of treatment used by women. There is no evidence that shaving can increase hair follicle density or size of the hair shaft. Plucking can be helpful if tolerated, but care must be taken to avoid folliculitis, pigmentation, and scarring.
Laser treatment has received more formal study than electrolysis as the primary mechanical method for removing excess hair and has been found to be an effective treatment in PCOS 86. Treatment removes hair because follicular melanin absorbs the laser wavelengths of light, which selectively thermally damage the target without damaging surrounding tissue. Women with dark hair and light skin are better candidates, and the approach appears to be most effective during anagen. Because of the skew of hair follicles among varying segments of the hair growth cycle, repeat treatments over time may be necessary 87. Concomitant medical management directed at decreasing androgen levels usually is recommended for excess androgen states, otherwise new vellus hairs will differentiate into terminal hairs, causing recurrence of hirsutism. The addition of eflornithine to laser treatment is superior in the treatment of hirsutism than laser alone 88.
Summary of Recommendations and Conclusions
-
▸ An increase in exercise combined with dietary change has consistently been shown to reduce diabetes risk comparable to or better than medication.
-
▸ Improving insulin sensitivity with insulin-sensitizing agents is associated with a decrease in circulating androgen levels, improved ovulation rate, and improved glucose tolerance.
-
▸ For women with PCOS, letrozole should be considered as first-line therapy for ovulation induction because of the increased live birth rate compared with clomiphene citrate.
-
▸ The addition of eflornithine to laser treatment is superior in the treatment of hirsutism than laser alone.
-
▸ Women with a diagnosis of PCOS should be screened for type 2 diabetes and impaired glucose tolerance with a fasting glucose level followed by a 2-hour glucose level after a 75-g glucose load.
-
▸ Women with PCOS should be screened for cardiovascular risk by determination of BMI, fasting lipid and lipoprotein levels, and metabolic syndrome risk factors.
-
▸ Reduction in body weight has been associated with improved pregnancy rates and decreased hirsutism, as well as improvements in glucose tolerance and lipid levels.
-
▸ There may be an increase in pregnancy rates by adding clomiphene citrate to metformin, particularly in obese women with PCOS.
-
▸ If clomiphene citrate or letrozole use fails to result in pregnancy, the recommended second-line intervention is either exogenous gonadotropins or laparoscopic ovarian surgery.
-
▸ Combination low-dose hormonal contraceptives are most frequently used for long-term management and are recommended as the primary treatment of menstrual disorders.
-
▸ Women in groups at higher risk of nonclassical congenital adrenal hyperplasia and a suspected diagnosis of PCOS should be screened to assess the 17-hydroxyprogesterone value.
-
▸ A low-dose regimen is recommended when using gonadotropins in women with PCOS.
-
▸ There is no clear primary treatment for hirsutism in PCOS.