Committee on Adolescent Health Care
This Committee Opinion was developed by the American College of Obstetricians and Gynecologists’ Committee on Adolescent Health Care in collaboration with committee members Geri D. Hewitt, MD and Karen R. Gerancher, MD.
Dysmenorrhea, or menstrual pain, is the most common menstrual symptom among adolescent girls and young women. Most adolescents experiencing dysmenorrhea have primary dysmenorrhea, defined as painful menstruation in the absence of pelvic pathology. When the patient’s history suggests primary dysmenorrhea, empiric treatment should be initiated. When a patient does not experience clinical improvement for her dysmenorrhea within 3–6 months of therapy initiation, her obstetrician–gynecologist should investigate for possible secondary causes and for treatment adherence. Secondary dysmenorrhea refers to painful menses due to pelvic pathology or a recognized medical condition. Endometriosis is the leading cause of secondary dysmenorrhea in adolescents. Endometriosis should be considered in patients with persistent, clinically significant dysmenorrhea despite treatment with hormonal agents and nonsteroidal antiinflammatory drugs, particularly if no other etiology for chronic pelvic pain or secondary dysmenorrhea has been identified based on history, physical examination, and pelvic ultrasonography. The appearance of endometriosis may be different in an adolescent than in an adult woman. In adolescents, endometriotic lesions are typically clear or red and can be difficult to identify for gynecologists unfamiliar with endometriosis in adolescents. Endometriosis in adolescents is considered a chronic disease with potential for progression if left untreated. The goals of therapy include symptom relief, suppression of disease progression, and protection of future fertility. Therapy must be individualized, and obstetrician–gynecologists should consider patient choice, the need for contraception, contraindications to hormone use, and potential adverse effects and counsel the adolescent and her family on treatment options.
Recommendations and Conclusions
The American College of Obstetricians and Gynecologists makes the following recommendations and conclusions:
-
Most adolescents experiencing dysmenorrhea have
primary dysmenorrhea, defined as painful menstruation in the absence of pelvic pathology. Primary dysmenorrhea characteristically begins when adolescents attain ovulatory cycles, usually within 6–12 months of menarche. -
Secondary dysmenorrhea refers to painful menses due to pelvic pathology or a recognized medical condition.
-
The most common cause of secondary dysmenorrhea is endometriosis.
-
Most adolescents who present with dysmenorrhea have primary dysmenorrhea and will respond well to empiric treatment with nonsteroidal anti-inflammatory drugs (NSAIDs) or hormonal suppression, or both. However, some patients either present initially with symptoms suggesting secondary dysmenorrhea or they fail empiric treatment for primary dysmenorrhea and require further evaluation.
-
Pelvic imaging with ultrasonography, regardless of findings on pelvic examination, also should be considered during evaluation for secondary dysmenorrhea.
-
Any obstructive anomaly of the reproductive tract, whether hymenal, vaginal, or müllerian, can cause secondary dysmenorrhea.
-
Although the true prevalence of endometriosis in adolescents is unknown, at least two thirds of adolescent girls with chronic pelvic pain or dysmenorrhea unresponsive to hormonal therapies and NSAIDs will be diagnosed with endometriosis at the time of diagnostic laparoscopy.
-
The appearance of endometriosis may be different in an adolescent than in an adult woman. In adolescents, endometriotic lesions are typically clear or red and can be difficult to identify for gynecologists unfamiliar with endometriosis in adolescents.
-
If a patient is undergoing a diagnostic laparoscopy for dysmenorrhea or chronic pain, or both, consideration should be given to placing a levonorgestrel-releasing intrauterine system (LNG-IUS) at the time of laparoscopy to minimize the pain of insertion.
-
Recommended treatment for endometriosis in adolescents is conservative surgical therapy for diagnosis and treatment combined with ongoing suppressive medical therapies to prevent endometrial proliferation.
-
Patients with endometriosis who have pain refractory to conservative surgical therapy and suppressive hormonal therapy often benefit from at least 6 months of gonadotropin-releasing hormone (GnRH) agonist therapy with add-back medicine.
-
Nonsteroidal antiinflammatory drugs should be the mainstay of pain relief for adolescents with endometriosis.
-
Adolescents should not be prescribed narcotics long-term to manage endometriosis outside of a specialized pain management team.
Background
Dysmenorrhea, or menstrual pain, is the most common menstrual symptom among adolescent girls and young women. Prevalence rates vary but range from 50% to 90% 1. Because of the high prevalence of dysmenorrhea in adolescents and the extent of its potential daily interference, obstetricians–gynecologists should be prepared to diagnose and treat this condition.
Definitions of Dysmenorrhea
Most adolescents experiencing dysmenorrhea have
Secondary dysmenorrhea refers to painful menses due to pelvic pathology or a recognized medical condition. The most common cause of secondary dysmenorrhea is endometriosis 56. Other causes of secondary dysmenorrhea include adenomyosis, infection, myomas, müllerian anomalies, obstructive reproductive tract anomalies, or ovarian cysts (see Box 1. In contrast to dysmenorrhea,
Box 1.
Causes of Secondary Dysmenorrhea
Reprinted from Harel Z. Dysmenorrhea in adolescents and young adults: an update on pharmacological treatments and management strategies. Expert Opin Pharmacother 2012;13:2157–70.
-
Endometriosis
-
Congenital obstructive müllerian malformations
-
Cervical stenosis
-
Ovarian cysts
-
Uterine polyps
-
Uterine leiomyomata
-
Adenomyosis
-
Pelvic inflammatory disease
-
Pelvic adhesions
Box 1.
Causes of Secondary Dysmenorrhea
Reprinted from Harel Z. Dysmenorrhea in adolescents and young adults: an update on pharmacological treatments and management strategies. Expert Opin Pharmacother 2012;13:2157–70.
-
Endometriosis
-
Congenital obstructive müllerian malformations
-
Cervical stenosis
-
Ovarian cysts
-
Uterine polyps
-
Uterine leiomyomata
-
Adenomyosis
-
Pelvic inflammatory disease
-
Pelvic adhesions
Box 2.
Metabolic Syndrome
The metabolic syndrome in women most commonly is diagnosed by the updated Adult Treatment Panel III criteria of an elevated blood pressure level (greater than or equal to 130/85), increased waist circumference (greater than or equal to 35 inches), elevated fasting glucose levels (greater than or equal to 100 mg/dL), reduced high-density lipoprotein cholesterol level (less than or equal to 50 mg/dL), and elevated triglyceride levels (greater than or equal to 150 mg/dL).
Data from Grundy SM, Cleeman JI, Dariels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute scientific statement: executive summary. Circulation 2005;112:e285–e290.
Box 1.
Suggested Evaluation for Patients With Polycystic Ovary Syndrome
Physical
Blood pressure
BMI (weight in kilograms divided by height in meters squared)
○ 25–30 = overweight, greater than 30 = obese
Waist circumference to determine body fat distribution
○ Value greater than 35 inches = abnormal
Presence of stigmata of hyperandrogenism and insulin resistance
○ Acne, hirsutism, androgenic alopecia, acanthosis nigricans
Laboratory
Documentation of biochemical hyperandrogenemia
○ Total testosterone and sex hormone-binding globulin or bioavailable and free testosterone
Exclusion of other causes of hyperandrogenism
○ Thyroid-stimulating hormone levels (thyroid dysfunction)
○ Prolactin (hyperprolactinemia)
○ 17-hydroxyprogesterone (nonclassical congenital adrenal hyperplasia due to 21 hydroxylase deficiency)
— Random normal level less than 4 ng/mL or morning fasting level less than 2 ng/mL
○ Consider screening for Cushing syndrome and other rare disorders such as acromegaly
Evaluation for metabolic abnormalities
○ Two-hour oral glucose tolerance test (fasting glucose less than 110 mg/dL = normal, 110–125 mg/dL = impaired, greater than 126 mg/dL = type 2 diabetes) followed by 75 g oral glucose ingestion and then 2-hour glucose level (less than 140 mg/dL = normal glucose tolerance, 140–199 mg/dL = impaired glucose tolerance, greater than 200 mg/dL = type 2 diabetes)
Fasting lipid and lipoprotein level (total cholesterol, high-density lipoproteins less than 50 mg/dL abnormal, triglycerides greater than 150 mg/dL abnormal [low-density lipoproteins usually calculated by Friedewald equation])
Ultrasound Examination
Determination of polycystic ovaries: in one or both ovaries, either 12 or more follicles measuring 2–9 mm in diameter, or increased ovarian volume (greater than 10 cm3). If there is a follicle greater than 10 mm in diameter, the scan should be repeated at a time of ovarian quiescence in order to calculate volume and area. The presence of one polycystic ovary is sufficient to provide the diagnosis.
Identification of endometrial abnormalities
Optional Tests to Consider
Gonadotropin determinations to determine cause of amenorrhea
Fasting insulin levels in younger women, those with severe stigmata of insulin resistance and hyperandrogenism, or those undergoing ovulation induction
Twenty-four hour urinary free-cortisol excretion test or a low–dose dexamethasone suppression test in women with late onset of polycystic ovary syndrome symptoms or stigmata of Cushing syndrome
Symptoms Associated With Dysmenorrhea
Several comorbidities significantly affect adolescents with dysmenorrhea and should be recognized by obstetrician–gynecologists. Symptoms associated with dysmenorrhea in adolescents may include nausea, vomiting, diarrhea, headaches, and muscle cramps 8. Poor sleep quality, including disturbances in sleep onset, latency, and sleep efficiency, has been self-reported by patients with severe dysmenorrhea compared with those with mild dysmenorrhea 9. As a result of these related symptoms, dysmenorrhea is the leading cause of recurrent short-term school absenteeism for adolescent girls 8. In one study, 12% of adolescent girls and young women aged 14–20 years lost days of school or work each month because of dysmenorrhea, and almost one in four respondents self-administered pain medication monthly without having seen a physician to investigate the cause of their pain 10. Notably, nearly two thirds of adolescents with chronic acyclic pain undergoing laparoscopy have endometriosis 11. In a 2015 study of adolescent girls (mean age 17.2) with laparoscopically diagnosed endometriosis, many presented with acyclic nonmenstrual pain, with 56% reporting a preoperative complaint of at least one gastrointestinal symptom, and 52% reporting at least one genitourinary symptom 12.
An association between premenstrual syndrome and dysmenorrhea in adolescent girls also has been demonstrated 13. A study of Japanese high school students showed that the rates of prevalence of premenstrual syndrome and premenstrual dysphoric disorder increased with the severity of dysmenorrhea 14. Furthermore, there is an increased risk of depression and anxiety in adolescents with dysmenorrhea 15. Health-related quality-of-life questionnaires administered to adolescents with dysmenorrhea have demonstrated the condition’s negative effect on physical and psychosocial functioning 16.
Evaluation of Primary Dysmenorrhea
Adolescents are particularly susceptible to delays in accessing medical care. They also may experience a longer time to diagnosis of pelvic pain (up to 5.4 years) compared with the time to diagnosis (1.9 years) in women whose symptoms began in adulthood 17. However, a delay in presentation, evaluation, diagnosis, and treatment is common for patients of all ages with dysmenorrhea. Barriers cited include difficulty with insurance coverage and a perceived lack of physician knowledge, time, or interest in chronic pain conditions 18.
The initial evaluation for all patients presenting with dysmenorrhea includes a medical, gynecologic, menstrual, family, and psychosocial history to determine whether the patient has primary dysmenorrhea or symptoms suggestive of secondary dysmenorrhea. When a patient presents with symptoms only of primary dysmenorrhea, a pelvic examination is not necessary. However, a pelvic examination should be conducted if symptoms of a sexually transmitted infection are present. Clinicians should suspect secondary dysmenorrhea if the patient reports severe dysmenorrhea immediately after menarche or progressively worsening dysmenorrhea, abnormal uterine bleeding (both heavy menstrual bleeding and irregular bleeding), mid-cycle or acyclic pain, infertility, lack of response to empiric medical treatment, family history of endometriosis, a renal anomaly, other congenital anomalies (spine, cardiac, or gastrointestinal), or dyspareunia. Furthermore, to minimize delays in diagnosis and treatment, obstetrician–gynecologists should be aware of cultural differences in attitudes about menstruation that may affect how comfortable a patient, particularly an adolescent, is with discussion of menstrual-related symptoms. Parental modeling also may play an important role in how a young patient reports and perceives pain as well as her anxiety about experiencing pain 19.
Management of Primary Dysmenorrhea
When the patient’s history suggests primary dysmenorrhea, empiric treatment should be initiated. Medical as well as complementary and alternative therapies are potential treatment options for the relief of pain.
Nonsteroidal Antiinflammatory Agents
Table 1.
Nonsteroidal Antiinflammatory Drugs Used During Menstruation in the Treatment of Primary Dysmenorrhea in Adolescents and Young Adults

Obstetrician–gynecologists should recommend NSAID dosage on an individual basis (see Table 1. Medication use is most effective when started 1–2 days before the onset of menses and continued through the first 2–3 days of bleeding 22. Taking the medication with food and increasing fluid intake may mitigate gastrointestinal and renal adverse effects. If one agent does not provide adequate relief, a different agent can be tried. Because children prescribed opioids for as few as 7 days can develop dependence that may lead to drug-specific withdrawal symptoms on abrupt discontinuation of the medications 23, opioids (including tramadol) should not be used as a treatment for dysmenorrhea. Hyperalgesia, a state of heightened pain sensitivity, also can result from repeated use of opioids and may lead to increasingly higher doses being prescribed 24. In addition to the risks of physical dependence and addiction, these effects make opioids an inappropriate treatment for adolescents with dysmenorrhea.
Because NSAIDs interrupt cyclooxygenase-mediated prostaglandin production, they are considered a first-line treatment option. Data show that NSAIDs are significantly better than placebo in providing pain relief from primary dysmenorrhea, although the superiority of any individual NSAID with regard to safety or efficacy has not been demonstrated 20. Because the prevalence of self-directed medication use in adolescents with dysmenorrhea is high 10 and the potential for sub-therapeutic treatment with incorrect interval dosage and timing is real, patient education is essential. A brief educational intervention can result in enhanced medication knowledge and a decrease in pain associated with dysmenorrhea 21. School personnel also should be educated about a student’s need to self-medicate while at school. Patients may need to provide authorization for medication use during school.
Hormonal Agents
If a trial of NSAIDs does not provide adequate relief of dysmenorrhea symptoms, consideration should be given to use of hormonal agents, which also are ideally suited as a first-line option. Nonsteroidal antiinflammatory drugs may be continued or added to hormonal therapy as needed. Several hormonal contraceptives are beneficial for the treatment of dysmenorrhea, including combined oral contraceptives, the contraceptive patch or vaginal ring, the single-rod contraceptive progestin implant, intramuscular or subcutaneous depot medroxyprogesterone acetate, and LNG-IUS 25. Each method has benefits and potential adverse effects and the decision to use one method over another should be patient driven. The mechanism of action for hormonal methods is likely related to prevention of endometrial proliferation or ovulation, or both, thus decreasing prostaglandin and leukotriene production 22. Compared with cyclic use of combined oral contraceptives, continuous regimens may result in a more rapid onset of pain reduction, but long-term success with both regimens is possible 26. Although not approved by the U.S. Food and Drug Administration for use as a contraceptive, continuous norethisterone acetate 5 mg (norethindrone) has been shown to be equally effective as a cyclic combined hormonal contraceptive, and data indicate it also decreases dysmenorrhea in women aged 18–23 years 1. Gonadotropin-releasing hormone agonists are not recommended for empiric use in patients with suspected primary dysmenorrhea because of concerns about their effect on bone mineral density 27.
Complementary and Alternative Therapies
Some patients and families seek complementary and alternative therapies. Adolescents should be asked about what alternative treatments they already may be using. There are promising, although limited, data on the benefits of exercise and heat treatment for the symptoms of dysmenorrhea 28. Given the low risk of harm and low cost of heat therapy and exercise, as well as the additional general health benefits of exercise, both options should be encouraged. Dietary supplements for which there may be limited evidence to suggest a potential benefit include fenugreek, ginger, valerian, zataria, zinc sulphate, fish oil, and vitamin B1 29. A recent study of adolescent girls with a mean age of 14.72 years demonstrated a decrease in the prevalence of dysmenorrhea when taking high-dose vitamin D weekly for 9 weeks 30; however, other studies show limited effect of vitamin D. Transcutaneous electrical nerve stimulation, acupuncture, herbal preparations, and yoga have demonstrated improvement in dysmenorrhea in some studies, but current evidence does not support them as first-line complementary and alternative therapies 22. Safety and efficacy data on herbal treatments are unclear.
Surgical Approaches to Management of Primary Dysmenorrhea
Surgical therapies have been proposed for primary dysmenorrhea. However, a systematic review found insufficient evidence to recommend the use of either uterine nerve ablation or presacral neurectomy for dysmenorrhea 31. Definitive and irreversible procedures such as ablation and hysterectomy should not be considered in adolescents.
Follow-Up for Primary Dysmenorrhea
Regardless of chosen therapy, patients with a presumed diagnosis of primary dysmenorrhea should be monitored for response to treatment. Response to treatment of primary dysmenorrhea supports the diagnosis. Tools that can be used for assessing dysmenorrhea at initial presentation as well as in response to treatment include visual analog scales and numerical rating scales. Both scales are reliable, valid, translated into the most frequently spoken languages, and are simple to administer and fulfill 32. When a patient does not experience clinical improvement for her dysmenorrhea within 3–6 months of therapy initiation, her obstetrician–gynecologist should investigate for possible secondary causes and for treatment adherence. Adolescents may be less adherent to medication schedules and may face conflict with parents about medication use. Other barriers may include forgetfulness, disorganization, financial costs, and pharmacy access. A literature review concluded that social support and peer relations were key themes in evaluating medication adherence, noting that adolescents worry about stigma and embarrassment in terms of social deviance, taking medications in front of peers, and having peers find out about their condition 33. An additional theme noted by the review was that medication nonadherence can be related to conflicts between adolescents and their parents. Such conflict could arise from parents who find it challenging to include the adolescent in the decision-making process, thus inhibiting self-management and the transition of treatment responsibilities, or conversely, from parents who show lack of support and involvement 33. Addressing these issues with patients and discussing methods to overcome such potential challenges may be helpful. After confirming treatment adherence, another hormonal method may be tried for an additional 3 months.
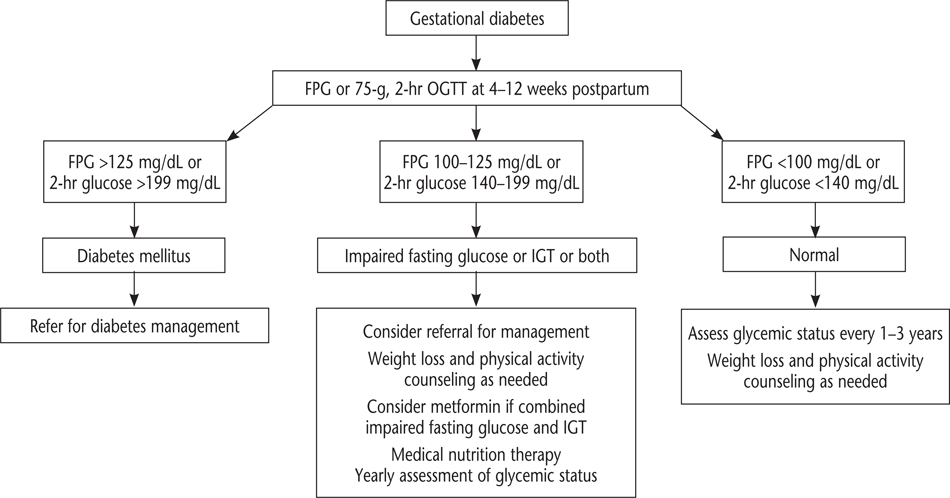
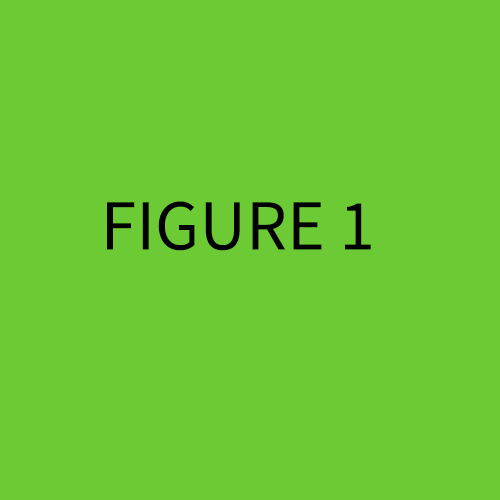
Evaluation of Suspected Secondary Dysmenorrhea
Most adolescents who present with dysmenorrhea have primary dysmenorrhea and will respond well to empiric treatment with NSAIDs, or hormonal suppression, or both 34. However, some patients either present initially with symptoms suggesting secondary dysmenorrhea or they fail empiric treatment for primary dysmenorrhea and require further evaluation (see Fig. 1. Additionally, if a patient has pain for 3–6 months, a more comprehensive evaluation of chronic pelvic pain should be performed with a history and focused physical examination to assess potential gastroenterologic, urologic, musculoskeletal, and psychosocial etiologies of pain.
Figure 1.
Approach to the adolescent with dysmenorrhea.

A pelvic examination to evaluate potential etiologies of secondary dysmenorrhea should be considered. With education and support, many adolescents who are not sexually active are able to tolerate a pelvic examination. Findings from a pelvic examination also may indicate other etiologies of secondary dysmenorrhea such as endometriosis, an obstructed reproductive tract anomaly, enlarged or irregularly shaped uterus, cervical friability or discharge (pelvic inflammatory disease), pelvic masses (ovarian cyst), vaginismus, or other pelvic floor disorders.
Pelvic imaging with ultrasonography, regardless of findings on pelvic examination, also should be considered during evaluation for secondary dysmenorrhea. Ultrasonography is the most appropriate initial imaging modality to identify potential etiologies of secondary dysmenorrhea, including obstructive reproductive tract anomalies, uterine myomas, and adnexal masses with endometriomas 35. Ultrasonography can be helpful in the diagnosis of ovarian endometriomas but is not useful for nonovarian endometriotic lesions 35. Although subsequent magnetic resonance imaging may be necessary to further delineate müllerian anomalies, it is not cost-effective as an initial screening tool 36. Although magnetic resonance imaging is likely to be equally as sensitive as ultrasonography in diagnosing ovarian endometriomas, it does not appear to be useful for identifying endometriotic peritoneal lesions or determining the extent of disease 36. A normal pelvic ultrasonography or physical examination does not eliminate the possibility of endometriosis.
Reproductive Tract Anomalies
Any obstructive anomaly of the reproductive tract, whether hymenal, vaginal, or müllerian, can cause secondary dysmenorrhea. The true incidence of reproductive tract anomalies is unknown, but they are estimated to occur in 0.1–3.8% of young women. Reproductive anomalies, both obstructive and nonobstructive, also are associated with endometriosis 37. Patients with urogenital sinus abnormalities and anorectal malformations are at increased risk of reproductive tract abnormalities and should be monitored for outflow tract obstructions as they progress through puberty and establish menses.
The goal of treatment in patients with obstructive reproductive tract anomalies is to establish a patent outflow tract to relieve symptoms and to decrease endometriosis and adhesions that can occur secondary to retrograde menses. Endometriosis associated with obstructive anomalies may improve after surgical correction and establishment of a patent outflow tract 37; however, persistent endometriosis after surgical correction of the obstructive anomaly has been reported 38.
Suspected Endometriosis
Endometriosis is the leading cause of secondary dysmenorrhea in adolescents. Endometriosis should be considered in patients with persistent, clinically significant dysmenorrhea despite treatment with hormonal agents and NSAIDs, particularly if no other etiology for chronic pelvic pain or secondary dysmenorrhea has been identified based on history, physical examination, and pelvic ultrasonography. Family history of endometriosis also should raise suspicion because patients with an affected first-degree relative have a 7-fold to 10-fold increased risk of developing endometriosis 39. To assess the effects of the symptoms on functionality in adolescents, it may be helpful to ask if they are missing school or participation in sports or other extracurricular activities.
Endometriosis is the most common finding in young women undergoing laparoscopy for chronic pelvic pain 6. Although the true prevalence of endometriosis in adolescents is unknown, at least two thirds of adolescent girls with chronic pelvic pain or dysmenorrhea unresponsive to hormonal therapies and NSAIDs will be diagnosed with endometriosis at the time of diagnostic laparoscopy.
Endometriosis remains a surgical and pathologic diagnosis in adolescents requiring the presence of endometrial glands and stroma in the biopsy specimen from a location outside of the endometrial cavity. Patients with persistent dysmenorrhea despite treatment and no other identified etiologies should be counseled about the high likelihood of endometriosis and the risks and benefits of diagnostic laparoscopy. The benefits of laparoscopy include confirmation of the presence or absence of endometriosis or other causes of chronic pain such as adhesive disease. Laparoscopy also presents an opportunity to treat endometriosis with coagulation, ablation, or resection of visible implants and adhesive disease with lysis of adhesions. Risks associated with laparoscopy include adverse effects from anesthesia, venous thromboembolism, bleeding, infection, wound infection, adhesion formation, and injury to surrounding structures. After shared decision making, some patients, together with their families and obstetrician–gynecologists, may opt for medical treatment of suspected endometriosis without having a confirmed pathologic diagnosis to avoid laparoscopy.
Laparoscopy for Endometriosis
The appearance of endometriosis may be different in an adolescent than in an adult woman. In adolescents, endometriotic lesions are typically clear or red and can be difficult to identify for gynecologists unfamiliar with endometriosis in adolescents Fig. 2, Fig. 3. Techniques described to enhance visualization of the lesions include moving the laparoscope within millimeters of the peritoneum (magnification technique) and filling the pelvis with saline and “diving in” with the laparoscope 27. Lesions suspicious of endometriosis should be sampled and biopsied, and visible lesions should be destroyed, ablated, or excised at the time of initial laparoscopy 27. Occasionally, biopsy of a suspicious lesion may not confirm endometriosis and visual diagnosis may suffice so that treatment can be initiated. The American College of Obstetricians and Gynecologists does not recommend “peritoneal stripping” in adolescents based on theoretical concerns (eg, adhesion formation contributing to bowel obstruction or infertility, or both, and persistent pain). In addition, there is a lack of short-term and long-term outcome data about the procedure.
Figure 2.
Red, inflamed adolescent endometriotic implant in the right paraovarian fossa. (Image courtesy of Geri Hewitt, MD, Nationwide Children’s Hospital, Columbus, Ohio.)

Figure 3.
Clear, vesicular adolescent endometriotic implant in the anterior peritoneum. (Image courtesy of Geri Hewitt, MD, Nationwide Children’s Hospital, Columbus, Ohio.)

At laparoscopy, most adolescents are diagnosed with early-stage endometriosis (American Society of Reproductive Medicine stage 1 or 2) 40, although there are a number of recent reports of young women presenting with more advanced disease 124142. When counseling families about surgical findings, it is important to communicate that the stage and location of endometriosis is not directly related to the frequency or severity of symptoms 43. Although typically diagnosed with earlier stage disease, adolescents may still experience substantial pain because the clear and red lesions are more metabolically active and are associated with greater prostaglandin production and subsequent pain and inflammation than the “powder burn” lesions seen in adult women 22.
If a patient is undergoing a diagnostic laparoscopy for dysmenorrhea or chronic pain, or both, consideration should be given to placing a LNG-IUS at the time of laparoscopy to minimize the pain of insertion. The LNG-IUS has been shown to decrease the pain associated with both dysmenorrhea unresponsive to oral contraceptive pills and dysmenorrhea and pain associated with endometriosis 44, although the LNG-IUS is not approved by the U.S. Food and Drug Administration for treatment of endometriosis-associated pain. Adolescents with endometriosis should not be treated with oophorectomy or hysterectomy.
Management of Endometriosis in Adolescents
Endometriosis in adolescents is considered a chronic disease with potential for progression if left untreated 45. The goals of therapy include symptom relief, suppression of disease progression, and protection of future fertility. There is no cure, nor is there a single best treatment option. Therapy must be individualized, and obstetrician–gynecologists should consider patient choice, the need for contraception, contraindications to hormone use, and potential adverse effects and counsel the adolescent and her family on treatment options.
Like endometriosis in adults, endometriosis in adolescents is considered an inflammatory-mediated estrogen-dependent disorder. Estrogen produced by the ovaries, as well as estrogen produced locally by the endometriotic implants due to aromatase activity, promotes increased prostaglandin production, resulting in pain 22. The recommended treatment for endometriosis in adolescents is conservative surgical therapy for diagnosis and treatment combined with ongoing suppressive medical therapies to prevent endometrial proliferation 27. First-line therapy for adolescents with either surgically diagnosed and destroyed endometriosis or presumed endometriosis includes suppressive hormonal therapy using a continuous combined hormonal contraceptive, a progestin-only agent, or 52 mg of LNG-IUS. All of these methods have been shown to be effective 46. Patients may benefit from trying several different types of hormonal suppression until they find their best fit. Because endometriosis is a chronic condition, patients should continue hormonal suppression unless they are actively trying to become pregnant.
Patients with endometriosis who have pain refractory to conservative surgical therapy and suppressive hormonal therapy often benefit from at least 6 months of GnRH agonist therapy with add-back medicine. Limited data exist regarding the long-term effects of GnRH agonist therapy on bone mineralization in adolescent patients. Leuprolide has been used in younger adolescents for the treatment of precocious puberty, obstructive anomalies, and for the care of transgender patients and those undergoing therapies for cancer. The obstetrician–gynecologist and patient should engage in a discussion of potential risks and benefits based on the patient’s individualized needs. Patients treated with GnRH agonists should begin add-back hormone therapy at the initiation of treatment to prevent bone loss and avoid the onset of menopausal symptoms. In a 2017 trial in adolescents, add-back therapy using a combination of conjugated equine estrogen (0.625 mg) and norethindrone acetate (5 mg) daily was superior to norethindrone acetate alone when comparing quality of life outcomes 47 and preservation of bone density 48. Dual-energy X-ray absorptiometry scanning is not needed before initiation of therapy, during GnRH agonist treatment of less than 12 months in duration, or after treatment. Obstetrician–gynecologists should counsel patients on adequate dietary calcium and vitamin D intake and the benefits of weight-bearing exercise during GnRH agonist therapy. After leuprolide is discontinued, patients should begin continuous hormone-suppression therapy.
Although serum CA 125 levels may be increased in patients with endometriosis, the American College of Obstetricians and Gynecologists does not endorse using CA 125 to monitor treatment or screen for endometriosis 49. Nonsteroidal antiinflammatory drugs should be the mainstay of pain relief for adolescents with endometriosis. Adolescents should not be prescribed narcotics long-term to manage endometriosis outside of a specialized pain management team.
Long-term Patient and Familial Education and Support
Adolescents with endometriosis often benefit from ongoing education and support and integration of other multidisciplinary services such as biofeedback, pain management teams, acupuncture, and herbal therapy 27. There is an absence of longitudinal data on fertility rates in adolescents with endometriosis, and early diagnosis and treatment may protect this population’s future fertility. The Endometriosis Foundation of America (www.endofound.org) and The Endometriosis Association (www.endometriosisassn.org) provide resources for adolescents and their families.